Care at the end of life
Care for people approaching the end of life is extremely important to us. Good palliative and supportive care allows people to die with dignity in a place of their choosing, without undue suffering. The experience of a patient's death will also live on in those they leave behind. We believe in providing as much support as possible to achieve a 'good' death.
Approximately 1% of the UK's population die each year, and within that population the majority of deaths can be predicted. Evidence has found that early identification of patients who are likely to die within the next 12 months often enables well coordinated, pro-active quality care and allows healthcare professionals to focus on better meeting patients' needs.
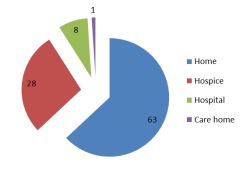
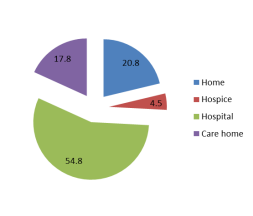
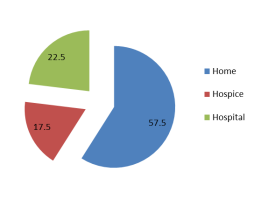
A National survey by Sue Ryder asked people where they preferred to die. The majority stated that their preferred place of death would be either a hospice or at home.
In 2015, Dr Brookes served as the Marie Curie and RCGP National Clinical Support Fellow for end of life care. Together with the RCGP, he developed an end of life toolkit, which contains resources for patients and those close to them, clinicians and commissioners. The palliative and end of life care toolkit provides a collection of tools, knowledge and current guidance to support patients nearing the end of life to live well until they die. We have also contributed to North Yorkshire County Council's Joint Strategic Needs Assessment for end of life care across the region.
The practice holds meetings every 4-6 weeks to discuss the care of patients in the last few months of life, whether this is through cancer, long term conditions such as COPD or frailty. The meetings are attended by the District Nursing team, Specialist Macmillan Nurses, Community rehab team, mental health specialists, our Community Matron and practice staff. Between us we can work together to provide the best possible care at this most challenging time for patients and those close to them.